
views
X
Expert Source
Kevin Stone, MDBoard Certified Orthopaedic Surgeon
Expert Interview. 19 November 2020.
You can spot EDS by certain tell-tale signs – to pinpoint the subtype, however, you may need a doctor’s help and genetic testing.
Finding Common Symptoms

Look for overly flexible joints. The most visible signs of EDS are shared among most of the six different subtypes. One is having overly flexible or “hypermobile” joints. This symptom can take a number of different forms, including joint “looseness” and the ability to extend joints past their normal range. It might also include joint pain and susceptibility to injuries. One giveaway that you have hypermobile joints is that you are able to extend the joints past their normal range of motion. Some people call this being “double-jointed.” Can you bend your little fingers back more than 90 degrees? Can you bend your elbows or knees backward? These are indications that you have “loose” joints. Besides being loose, the joints may be unstable and prone to dislocate. Someone with EDS may also suffer from chronic joint pain or develop early onset osteoarthritis.

Note stretchy skin. People with EDS often have distinctive skin, too. The body’s weakened connective tissues let the skin stretch more than it normally would and the skin usually appears very soft and shiny. The skin is also highly elastic and will spring back into place if stretched. Keep in mind that some people with EDS display hypermobile joints but not these skin symptoms. Is the skin exceptionally soft, thin, elastic, or loose? These are potential signs of a number of medical complications, including EDS. Try the following test: pinch a small area of skin on the back of the hand and gently pull up. For people with typical skin symptoms of EDS, the skin will immediately snap back into place.

Beware of fragile skin and easy wounding. Another related sign of EDS is that the skin is very fragile and prone to wounding. Skin can bruise or even split easily and will take longer than usual to heal. People who are affected may also develop severe scarring over time. Do you bruise at the slightest bump? Because the connective tissue is weak, people with EDS may easily bruise, break blood vessels, or experience prolonged bleeding after a trauma. You may also need to be tested for prothrombin blood clotting, another potential cause of easy bruising. For someone with EDS, the skin may be fragile enough to tear or break open with very slight force. It may also take a long time to heal. For instance, stitches meant to close a wound may tear out and leave a large scar. Many people with EDS have distinct scarring that is described as looking like “parchment” or “cigarette paper.” These scars are long and thin and form where the skin has split open.
Identifying Subtypes of the Syndrome

Note indications of hypermobility. “Hypermobility” is the least serious of all EDS subtypes but can still have major effects, especially on the muscles and skeleton. The biggest indication of this subtype is joint hypermobility. However, there may be additional signs in addition to the shared symptoms above. Apart from joint looseness, many people with the hypermobility subtype can suffer frequent dislocations of the shoulder or patella with little or no trauma and a good deal of pain. They may also develop diseases like osteoarthritis. Chronic pain is a primary sign of hypermobility EDS, too. This pain can be severe – “physically and psychologically disabling” – and can’t always be accounted for. Doctors are not sure, but it may come from muscle spasms or arthritis.

Read signs for the “classical” subtype. The “classical” version of EDS usually shows the common skin and joint symptoms, i.e. the skin is fragile and the joints are overly mobile. However, there are other symptoms that are associated with this subtype. These should be considered when trying to reach a diagnosis. People with this subtype of EDS often have scars over pressure points like the knees, elbows, forehead, and chin. The scars at these locations may also have hardened, calcified bruises. Some people also develop “spheroids” on the forearms or shins. These are small cysts under the skin that contain fat and are movable. People with this subtype of EDS may also have poor muscle tone, fatigue, and muscle cramps. In some cases, they may suffer from hiatal hernias or even anal prolapse.
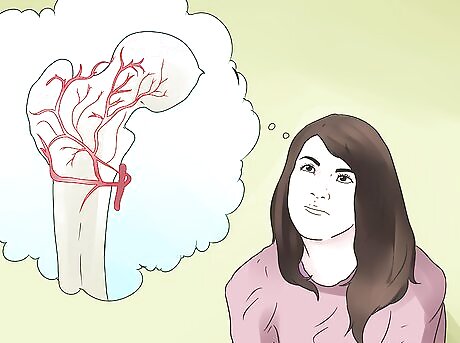
Look for vascular complications. Vascular EDS is the most dangerous subtype, because it affects the internal organs and can lead to things like internal bleeding or even death. More than 80% of people with this subtype experience a complication by age 40. People with vascular EDS often have a certain physical appearance. This includes thin and translucent skin, which is most visible on the chest. They may also be short with thin hair, and have large eyes, a thin nose, and ears without lobes. Other signs of vascular EDS are clubfoot, joint looseness limited only to the fingers and toes, premature skin aging on the hands and feet, and early varicose veins. The most serious signs for this subtype have to do with internal injuries. Bruising is very easy. Vascular EDS can also lead arteries to rupture or collapse without warning. This is the leading cause of death for those with this subtype.
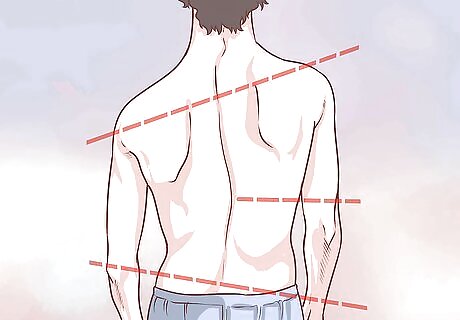
Observe signs of scoliosis. Another form of EDS is the Kyphoscoliosis subtype. The main feature of this kind is the sideways curvature of the spine (scoliosis). Kyphoscoliosis EDS can show itself at birth in this as well as other major symptoms. As said, look for lateral curvature of the spine. In kyphoscoliosis EDS, scoliosis is present at birth or within the first year and is progressive, meaning it gets worse over time. Often, people with this subtype are unable to independently in adulthood. People with the Kyphoscoliosis subtype also usually have severe joint looseness and poor muscle tone at birth. This can delay the child’s motor skills. Another sign has to do with the eyes. The Kyphoscoliosis subtype weakens the whites of the eye or sclera.

Watch out for hip dislocations. The main sign of the arthrochalasia subtype is the frequent dislocation of the hips starting from birth. Along with skin elasticity, easy bruising, and fragile tissue, this sign is present in all people with this variety of EDS. Arthrochalasia EDS is mainly identified by frequent dislocations and displacements of the hip joints. However, it can also include poor muscle toning and scoliosis.

Pay closer attention to the skin. The last and least common variety of EDS is the dermatosparaxis subtype, which is named after symptoms related to the skin. People with this kind of EDS have more fragile skin and severe bruising than others but otherwise different features. Note the skin’s appearance. In Dermatosparaxis EDS, the skin is soft and doughy and there is less elasticity. Many people have excess and sagging skin, especially around the face. People with Dermatosparaxis EDS may be prone to large hernias. However, they have skin that heals normally and do not scar as in other subtypes.
Confirming the Diagnosis

Talk to a doctor. If you think that you or a loved one might have EDS, talk about your concerns with a physician. Your regular doctor may be able to advise you but will more likely refer you to a specialist in genetic diseases. Expect a series of questions about medical and family histories, a thorough exam, and a blood test. Set up an appointment. Before you see the doctor, think about what symptoms you have seen or experienced. The doctor may ask if your or your loved one’s joints are overly flexible, if the skin is stretchy, or if the skin heals poorly. She will also probably ask about any medications the patient is taking.

Look for a family connection. Since EDS is a genetic syndrome, it gets passed down in families. This means that you or a loved one is more likely to have the mutations if a close family member had them, as well. Think carefully and be prepared to answer questions about your family history. Did any of your or your loved one’s relatives have a diagnosed case of EDS? Or, did they have symptoms like the ones you’re seeing? Do you know of any relatives who died suddenly from a ruptured blood vessel or organ? Recall that this is one of the most serious complications of vascular EDS and may indicate an undiagnosed case. Your doctor will try to diagnose by type, finding the EDS subtype that most closely matches the patient’s symptoms.
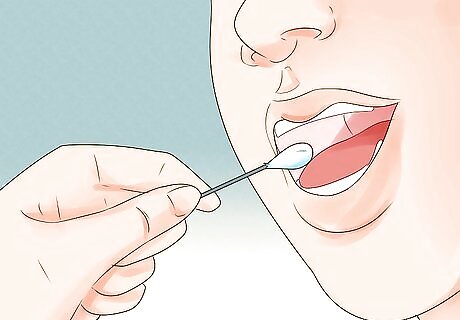
Have genetic testing. Usually a specialist can make a diagnosis on the basis of the skin, joints, and a family history. However, they can also use genetic tests to confirm EDS or the specific subtype that is present. A DNA test can pinpoint the problem and show the specific genes that are mutated. Genetic testing can be done to confirm Vascular, kyphoscoliosis, Arthrochalasia, Dermatosparaxis, and sometimes Classical EDS. For testing, expect to be referred to a clinical geneticist or genetic counselor. You’ll then give a sample of either blood, saliva, or skin for laboratory testing. Genetic tests are not always 100% accurate. Some people recommend that they be done conservatively to confirm rather than rule out a diagnosis.




















Comments
0 comment