
views
X
Trustworthy Source
PubMed Central
Journal archive from the U.S. National Institutes of Health
Go to source
Some mild hallucinations might be successfully treated at home, but severe or chronic hallucinations will always require professional help.
Home Management (Self Care)

Understand the nature of hallucinations. Hallucinations can affect any of your five senses—sight, hearing, taste, smell, or touch—and they can be caused by numerous underlying conditions. The perceptions must occur during a state of consciousness, however, and they will seem very real. Most hallucinations are disorienting and cause distress in those experiencing them, but some can seem pleasant or enjoyable. Hearing voices qualifies as an auditory hallucination, while seeing lights, people, or objects that aren't really there is a common visual hallucination. The sensation of "insects" or other objects crawling on the skin is a common hallucination of touch.
Check for a fever. High fevers have been known to cause hallucinations of all degrees, especially in children and the elderly. Even if you do not fall into either demographic, fever can still be a cause of some hallucinations, so it is worth checking for. Hallucinations can occur with any fever higher than 101 degrees Fahrenheit (38.3 degrees Celsius), but they are more common when dealing with fevers higher than 104 degrees Fahrenheit (40 degrees Celsius). Any fever higher than 104 degrees Fahrenheit (40 degrees Celsius) warrants immediate medical attention, regardless of whether or not it is accompanied by hallucinations. For fevers you can treat at home, begin by taking a fever-reducing medication like ibuprofen or acetaminophen. Drink plenty of fluids and monitor your temperature regularly.

Sleep better. Mild and moderate hallucinations can be caused by severe sleep deprivation. Severe hallucinations are generally caused by other conditions but can be aggravated by sleep deprivation, as well. The average adult should receive between seven and nine hours of sleep every night. If you are currently suffering from severe sleep deprivation, you may need to temporarily increase this amount by several hours until your body recovers. Sleeping during the day can disturb your usual sleep cycle and may trigger insomnia and hallucinations as a result. If your sleeping patterns are thrown off, you should try to establish a normal sleep pattern.

Manage stress more effectively. Anxiety is another common cause of mild to moderate hallucinations, and it can also worsen severe hallucinations caused by other factors. As such, learning to minimize mental and physical stress can help reduce the frequency and severity of your hallucinations. Reduce physical stress by keeping yourself hydrated and well-rested. Regular light to moderate exercise can also improve your overall health and relieve your body of stress-related symptoms, including mild hallucinations.

Know when to call for help. If you are unable to distinguish reality from hallucination, you should seek immediate emergency medical care. You should also schedule an appointment with your doctor if you experience mild hallucinations on a frequent basis, since they are probably caused by an underlying medical condition. This is especially true if taking general home measures to improve your health have no effect. If you experience hallucinations that are accompanied by other severe symptoms, you should also seek emergency medical care. Such symptoms include discolored lips or fingernails, chest pain, clammy skin, confusion, loss of consciousness, high fever, vomiting, abnormal pulse, breathing difficulties, injury, seizure, severe abdominal pain, or irrational behavior.
Home Management (External Care)

Know the signs. People who experience hallucinations may not openly talk about what they sense. In these instances, you will need to know how to identify less obvious signs of hallucination. Someone with auditory hallucinations may seem unaware of his or her surroundings and may excessively talk to himself or herself. That individual may seek isolation or obsessively listen to music in an attempt to drown out the voices. Someone who visually fixates on something you cannot see might be experiencing a visual hallucination. Scratching or brushing away seemingly invisible disturbances can be a sign of tactile hallucinations, while holding one's nose can indicate smell-based hallucinations. Spitting food out can be a sign of taste-based hallucinations.
Stay calm. If you need to treat or help someone else suffering from hallucinations, it is important to remain calm throughout the entire process. Hallucinations can become sources of severe anxiety, so the patient might already be in a state of panic. Adding more stress and panic to the situation will only worsen things. When someone you know suffers from frequent hallucinations, you should also discuss what happens during a time when he or she is not actively hallucinating. Ask about what is most likely to occur and what the patient needs you to do to offer support.
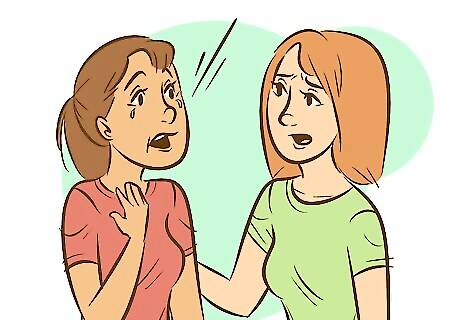
Explain the reality. Calmly explain to the patient that you are unable to see, hear, feel, taste, or touch the sensation he or she is describing. Explain this in a straightforward and non-accusatory manner to avoid upsetting the patient. If the hallucinations are mild to moderate, and if the patient has had past episodes of hallucinations, you may also try to explain that the sensations he or she is experiencing are not real. Patients who experience hallucinations for the first time or those with severe hallucinations may not be able to understand that they are hallucinating, however, and may lash out if they are questioned or doubted.
Distract the patient. Depending on the circumstances, it might be helpful to distract the patient by switching topics of conversation or by physically moving to a different location. This is especially true of mild to moderate hallucinations, but you may not be able to reason with patients experiencing severe hallucinations.

Encourage the patient to seek professional help. If you know someone who suffers from frequent hallucinations, you should strongly encourage that individual to seek professional medical or psychological help. Talk with the patient when he or she is not actively experiencing a hallucination. Discuss the severity of the situation and share any knowledge you have on potential causes and solutions. Approach the situation from a position of support and love, though, and never from an accusatory standpoint.
Monitor the situation. When hallucinations escalate in severity, they can become a safety threat to the person experiencing them or to others around that individual. When safety is an issue, you should call for emergency medical help. If hallucinations are accompanied by other severe physical symptoms, or if they are so severe that the patient can no longer separate fiction from reality, you should also seek emergency medical care.
Medical Treatment
Diagnose and treat the underlying cause. Hallucinations are typically symptomatic of certain psychiatric disorders, but some physiological medical conditions can cause hallucinations, too. The only way to fix the hallucinations long-term is to treat the underlying condition causing them. Psychological conditions that can cause hallucinations include schizophrenia, schizoid or schizotypal personality disorders, psychotic depression, post-traumatic stress disorder, and bipolar disorder. Physiological conditions that impact the central nervous system can cause hallucinations, as well. These can include brain tumors, delirium, dementia, epilepsy, stroke, and Parkinson's disease. Certain infections, like bladder infections or chest infections, may also cause hallucinations. Migraines can cause hallucinations in some individuals, too. Drug or alcohol abuse can cause hallucinations, too, especially when consumed in high quantities or during periods of withdrawal.

Take antipsychotic medication. Antipsychotics, also known as neuroleptic drugs, can control hallucinations in most circumstances. These drugs can be prescribed to help treat hallucinations caused by both psychological and physiological conditions, especially when other treatments are unavailable or not enough. Clozapine, an atypical neuroleptic, is normally given in doses between 6 to 50 mg per day depending on the severity of the hallucinations. The dosage must be increased slowly to prevent fatigue. Regular white blood cell tests must be taken while on this medication, however, since it can lower white blood cell counts to dangerous levels. Quetiapine is another atypical neuroleptic that can treat hallucinations. It is generally less effective than clozapine in most circumstances, but it is also fairly safe to use for most underlying conditions. Other common antipsychotics include risperidone, aripiprazole, olanzapine, and ziprasidone. These medications are generally well tolerated by most patients, but may not be safe for patients suffering with Parkinson's disease.

Adjust dosages of current prescription medications. Some medications used to treat other conditions can cause hallucinations in some individuals. This is an especially common occurrence among patients with Parkinson's disease. Even if you suspect that medications might be causing your hallucinations, you should never stop any drug without first talking to your doctor. Suddenly stopping a medication can cause other complications. In the case of Parkinson's patients, amantadine and other anticholinergic medications are typically stopped first. If this does not help, dopamine agonists might be lowered to a smaller dosage or stopped entirely. When controlling these medications does not control a patient's hallucinations, doctors may still prescribe an antipsychotic drug. This is also the case when lowering the dosage of these medications causes other Parkinson's symptoms to return or worsen.

Enter rehabilitation, if necessary. If you're addicted to hallucination-inducing drugs or alcohol, you should check into a rehabilitation program to help you recover from your addiction. Cocaine, LSD, amphetamines, marijuana, heroin, ketamine, PCP, and ecstasy can all cause hallucinations. While some drugs can cause hallucinations, quitting the substance too suddenly can cause hallucinations to develop, too. Hallucinations caused by withdrawal can usually be controlled with antipsychotic medications, though.

Attend regular therapy. Cognitive behavioral therapy, in particular, can help some patients who suffer from frequent hallucinations, especially when those hallucinations are caused by psychological disorders. This type of therapy evaluates and monitors the patient's perceptions and beliefs. By identifying possible psychological triggers, a professional psychologist might be able to construct strategies that allow the patient to cope with and reduce symptoms.

Seek a support group. Both support groups and self-help groups can minimize severity and frequency of hallucinations, especially when those hallucinations are auditory and caused by psychological triggers. Support groups provide patients with a way to plant themselves firmly in reality, thereby helping them to separate false hallucinations from real life. Self-help groups encourage people to accept responsibility over their hallucinations in a manner that encourages them to control and cope with those hallucinations.



















Comments
0 comment