
views
It’s important to remain vigilant and take precautions against Mpox, which may not be as lethal as Covid-19 but must not be ignored, experts have told News18.
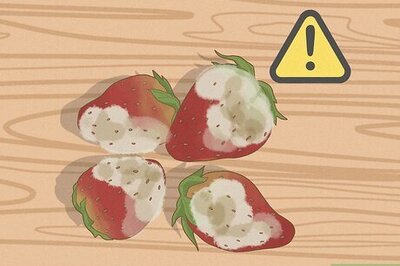
Experts said public must understand that they should not fear but also should not hide lesions or blisters on the skin — the most noticeable symptoms of Mpox or monkeypox infection.
India, which has seen no cases so far, has already increased its surveillance following the alert by the World Health Organization (WHO) about the surging number of Mpox cases in various parts of the world, especially the Democratic Republic of the Congo (DRC).
“There is no need to panic. Going by the data, in the last two years, we have seen around one lakh cases globally. India has seen around 30 cases in the previous two years which is not a big number. Still, we must understand that there is no margin for complacency when we are dealing with a virus,” former Indian Council of Medical Research (ICMR) scientist Dr Raman Gangakhedkar told News18.
He advised that if one notices skin lesions or boils, “don’t hide and don’t fear”.
“The death rate is low. The infected person only needs to be isolated for three to four weeks most often. If one follows barrier nursing, there is a very small risk of acquiring infection while providing care to an infected individual,” said Gangakhedkar, the country’s top epidemiologist.
He said people who have taken doses of smallpox vaccines are likely to be safe from Mpox infection. “Smallpox shots were last given in 1978-79 — it means the population over 45 years old that got this shot is assumed to be safe from the Mpox virus. Also, in Congo, the infection has been reported among pregnant women.”
Does the new variant pose a high risk?
According to Dr Anurag Agrawal, dean, biosciences and health research at Trivedi School of Biosciences, Ashoka University, there was a similar warning in 2022 after a global outbreak, which was withdrawn after new cases rapidly fell in 2023.
He explained that “Clade I, seen in the Congo basin, had less human-to-human spread but led to a higher rate of severe infections and death. Clade II, seen in West Africa, had a greater spread but infections were less severe. “
The large international surge starting July 2022, primarily driven by sexual contact amongst men, was due to Clade IIb, with even lower virulence. The 2022 MPox outbreak was thus mostly a self-limited disease, with low mortality rates.
“Despite this, there were about 200 deaths, mostly in countries that had never reported Mpox before,” he pointed out, adding that “the current outbreak seems different”.
Raising an important point, Agrawal highlighted that it is Clade I, “with likely higher mortality”. “Cases are being reported from multiple countries neighbouring Democratic Republic of the Congo (DRC) and most of the deaths are in children, raising fear of non-sexual human-to-human transmission.”
“While there is no clear evidence of respiratory transmission, there is fear that the virus is evolving,” said Agrawal, who is former director of the Institute of Genomics and Integrative Biology, a national laboratory of CSIR.
“Smallpox could be transmitted via the respiratory route, making it a dreaded pandemic. Every new infection is an opportunity for the virus to evolve, as we learnt during the SARS-CoV-2 pandemic. Efforts must thus be directed towards containing the ongoing spread of MPox.”
Similarly, Dr Gangakhedkar, pointed out that in Congo, the infection has been reported among pregnant women as well. “Also, there is a fear that 1B can be transmitted sexually and hence, it can spread like any other sexually transmitted infection.”
On the positive side, he pointed out that one thing about Clade 1B that can help in controlling its spread is the appearance of lesions on the general body such as near the mouth, unlike in Clade IIb where blisters appear around the genitals in adults. However, the skin lesions occur in non-genital regions in children. “This can help during physical screening at airports as these blisters or lesions are unlikely to be missed.”
Can Mpox infect humans via animals?
Emphasising the need to adopt the ‘One Health’ approach, Dr Vishal Rao, a member of Karnataka’s genomic surveillance committee quoted the criteria and definition of “monkeypox” infection in 2003 by the American health watchdog, Centers for Disease Control and Prevention (CDC).
The criteria included the interaction of patients with “exotic mammalian pets” with clinical signs of illness such as conjunctivitis, respiratory symptoms or rash.
In the outbreak of 2003, people in Illinois, Indiana and New Jersey were found to have human monkeypox. All of the individuals, ranging in age from four to 48 years, had contact with ill prairie dogs purchased as pets from exotic pet stores.
Rao, who is also the dean for the Centre of Academic Research at Bengaluru-based HCG Cancer Hospital, advised that India strengthen surveillance mechanisms over the environment, humans and animals.
“While Covid-19 was caused by droplets, Mpox is caused by touch. We need to stay vigilant. We have paid the price with Covid-19 but now, we have a system of genomic surveillance in place which can be very beneficial.”
















Comments
0 comment