
views
X
Research source
Akiva J Marcus MD, B.S Anand ,Chronic Gastric, emedicine/medscape Dec 19 2014
Though gastritis usually improves with treatment, ulcers can increase your risk of stomach cancers.[2]
X
Trustworthy Source
Mayo Clinic
Educational website from one of the world's leading hospitals
Go to source
It's important to recognize the symptoms of gastritis so you can get early treatment, relieve your symptoms and prevent complications.
Recognizing the Symptoms of Gastritis

Take note of abdominal pain. Patients with gastritis often experience "epigastric pain," or pain in the upper central abdomen. It can be described as a burning, gnawing, or deep boring pain. You may find that it wakes you up in the middle of the night, but it can often be relieved by eating something or taking an antacid.

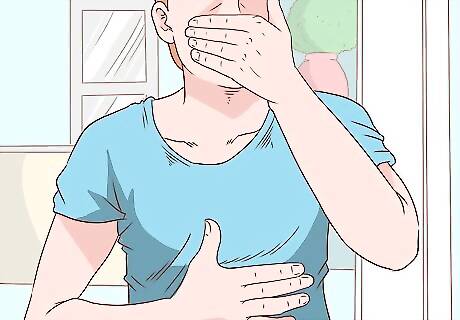
Look for nausea and vomiting. These symptoms are fairly common with gastritis. You may also see blood or bile in your vomit. The blood may be partially digested and look like coffee grounds. This is caused by bleeding ulcers. You should contact a doctor immediately if you see blood or green bile in your vomit. Excessive vomiting can often lead to dehydration, which can also be dangerous. Make sure to get a lot of fluids if you're vomiting.

Check for black, tarry stool. The black, tarry stool seen in many gastritis patients is called “melena.” The same bleeding ulcers that make people vomit blood causes them to excrete it through stool. This should also be reported to the doctor as soon as possible.
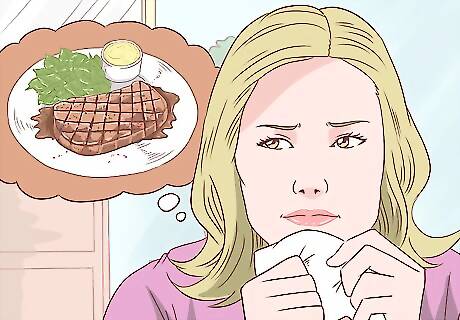
Be aware of a change in appetite. People with gastritis often find that they've lost their appetite. You may lose it altogether or simply find that you feel full after a smaller amount of food than usual. Take notice if your clothes feel unusually loose without any explanation. If you're losing weight without purposely dieting, you may be eating less. If your appetite decreases significantly, you may eat little enough to be considered anorexic. See a doctor if you feel woozy or dizzy from a lack of nutrition or fluids.
Notice excessive burping and bloating. The inflammation in the stomach lining causes gases to build up. This, in turn, can make you belch more than you usually would. Even with the release of gas through burping, you may still feel bloated from all the gas that’s trapped in your stomach.
Getting Diagnosed

See a doctor for a physical exam. Let the doctor know that you suspect gastritis, and ask him to focus on an abdominal exam. Bring a prepared list of all the symptoms you’ve experienced and show it to your doctor. He will look for “alarm symptoms” that suggest you need urgent care. The alarm symptoms you should make sure to tell the doctor about are: Vomiting blood or bile Black tarry stool (melena) Appetite loss, anorexia, and weight loss (especially of six pounds or more) Anemia (this may cause you to be pale, tired, weak, or dizzy) A bulge you can feel in your abdomen Let the doctor know if you are over 55 years old, as well.
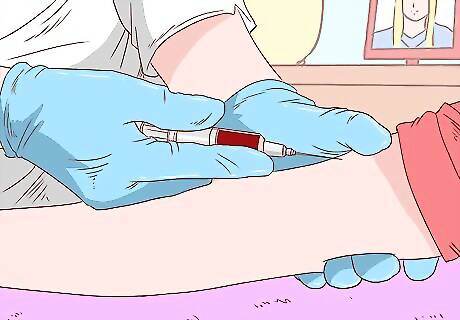
Allow the doctor to take a blood sample. Once the sample has been drawn, he will send it to the medical lab for analysis. The lab may run the following tests: Complete Blood Count (CBC) to check for anemia Amylase and Lipase to rule out pancreatic disease Liver function test and renal function test to assess for dehydration and for other causes of your symptoms if you’re vomiting Stool guaiac test for occult blood (not visible in the stool) A urea breath test or stool/blood test to check for the bacteria Helicobacter Pylori
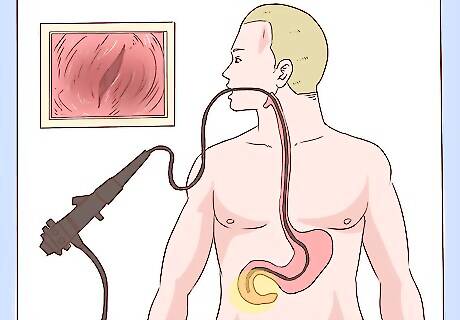
Be prepared for an endoscopy if you have "alarm symptoms." If the doctor is worried about the list of symptoms you've provided, he will likely order an endoscopy for you. He will insert a small camera attached to a long, flexible tube down your throat. The camera will reach far enough down to observe the esophagus, stomach, and part of the small intestine. If you tested negative for H. Pylori, but continue to have symptoms, you may choose to have an elective endoscopy. You can ask for a sedative during the procedure to help you relax. While you may feel pressure, you won’t feel any pain. The doctor will look for ulcers, erosions, tumors, and other abnormalities. He can also take biopsies to be tested in the lab.
Eradicating the H. Pyloria Bacteria
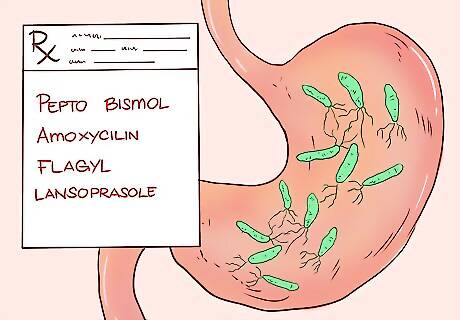
Take medication to fight the H. Pylori bacteria. If your gastritis is caused by this bacteria, your doctor will prescribe medication to kill it. The first “eradication protocol” for addressing this bacteria has a 90% success rate. Your doctor may prescribe four medications to be taken for one day: Pepto Bismol: 525 mg taken orally four times Amoxicillin: 2 g taken four times Flagyl: 500 mg taken orally four times Lansoprasole: 60 mg taken orally once
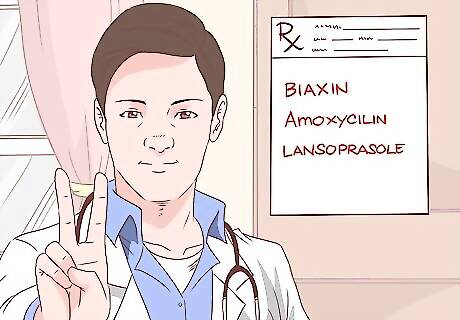
Proceed to the second “eradication protocol” if necessary. If the initial treatment does not successfully kill off the H. Pylori bacteria or if your doctor feels that you should do so, your doctor may prescribe a second round. The combination of medications in this protocol have an 85% success rate at killing the bacteria: Biaxin: 500 mg taken orally twice daily for seven days Amoxicillin: 1 g taken orally twice daily for seven days Lansoprazole: 30 mg taken twice daily for seven days

Expect longer treatment for children. Shorter, more intense treatments are not recommended for children. Not enough studies have been done to research the effects on their bodies. Instead, the doctor will recommend a longer two-week regimen. Their medication will also be prescribed in divided doses. For example, a divided dose of 50 mg/kg per day means you give the child 25 mg/kg twice during the course of the day. Amoxicillin: 50 mg/kg in divided doses twice daily for 14 days. Biaxin: 15 mg/kg in divided doses twice daily for 14 days. Omeprazole: 1 mg/kg divided twice daily for 14 days.
Relieving the Symptoms

Learn the goal of supportive treatment. If you didn’t have the H. Pylori bacteria or after it’s been addressed, the remaining treatment for gastritis is “supportive.” This means that its goal is to relieve symptoms.
Reduce your stress levels. Gastritis can be caused by severe stress related to major surgery, injury, burns or severe infections. Lowering your stress may help with your gastritis.
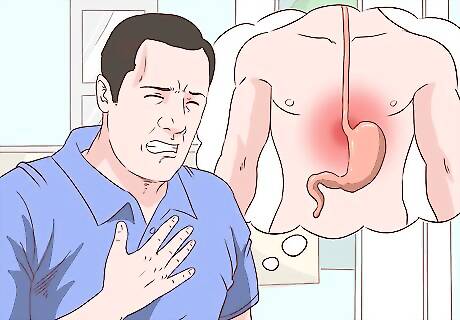
Treat any heartburn you experience. People have different experiences of heartburn. Some may feel a mild burning while others have pain so severe it feels like a heart attack. Heartburn is the result of stomach acid getting up into the esophagus where it doesn't belong. This is often the result of a loose gastroesophageal sphincter. If you overeat, you can apply too much pressure on this sphincter, forcing your stomach contents up past it. Heartburn can also be caused by simple gravity. When you lie down right after a meal, you encourage stomach fluid to flow up into the esophagus. The first line of treatment for heartburn is with proton pump inhibitors (PPI). The doctor may prescribe Lansoprazole or Omeprazole. The second line of treatment is with H-2 blockers like Pepcid or Zantac.
Discontinue behaviors that cause Peptic Ulcer Disease (PUD). If you take non-steroidal anti-inflammatory drugs (NSAIDs) for pain, they may be causing your ulcers. Examples of NSAIDs include aspirin and ibuprofen. Talk to your doctor about finding an alternative treatment to manage your pain. Smoking and drinking alcohol can also put you at greater risk of peptic ulcers. Avoid herbal products and supplements, as they may worsen your condition. Ask your doctor if your current medications, like bisphosphonates to treat osteoporosis, may be the culprit. Figure out an alternative course of treatment if so.

Take PPIs to treat PUD. Peptic Ulcer disease has been on the decline since the advent of PPI therapy. PUD can cause gnawing, burning, or boring pain in the upper abdomen. If you have no "alarm symptoms," you'll usually take PPIs to neutralize the acid eroding your stomach lining. Possible prescription options include Nexium, Vimovo, Prevacid, Prilosec, Zegerid, and Aciphex.

Turn to surgical remedies if necessary. Most ulcers are found in the stomach and duodenum (the first part of the small intestine). If PPI therapy doesn't help your symptoms, talk to your doctor about your surgical options. Though the procedure is less common now than it once was, the doctor may suggest a vagotomy. In a vagotomy, a surgeon severs branches of the vagus nerve that are responsible for producing stomach acid.
Get treatment for nausea and vomiting. If nausea and vomiting are part of gastritis, then the gastritis needs to be treated to avoid complications like ulcers and cancer. You will likely undergo antiemetic therapy. Antiemetic drugs are used to control nausea and vomiting. You might get a shot of Zofran or take a tablet that diffuses the medication under your tongue. If you've been vomiting a lot, you may be dehydrated. In that case, you may receive IV hydration. Tell the doctor if you feel dizzy or weak after vomiting, if you are urinating less than usual or your urine is very dark, or if it takes longer than usual for your skin to snap back when you pull it.

Eat smaller meals to control gas. If your major symptoms are bloating and belching, unfortunately, as of now, there's no good therapy available to treat these symptoms. The best you can do is to eat smaller, but more frequent meals throughout the day. You get the same amount of nutrition, but put less strain on your digestive system. Anti-gas medications like simethicone could be tried for belching and bloating due to gas.



















Comments
0 comment