
views
Transmasculine Top Surgery

Be prepared to stay in the hospital overnight. Most of the time, transmasculine top surgery (meaning the removal of breasts to create a masculine chest) is an outpatient surgery, meaning that you will go home or to wherever you will recover locally after the procedure. Sometimes, you might need to spend at least 1 night in the hospital so you can rest and your medical team can make sure you’re recovering well. Ask your surgeon how long they expect your hospital stay to be. If they think you’ll be there for 1 or more nights, pack a hospital bag with supplies such as your toothbrush and hairbrush, slippers, comfortable clothing, your phone charger, and something to keep you entertained. Although it varies according to the specific procedure and incision type, your surgery will probably last somewhere between 1-4 hours. Transmasculine top surgery involves removing the glandular tissue and fat from inside your breasts to make them smaller. If your breasts are large, your surgeon might also need to remove and resize your nipples and areolas and then graft them back on. This procedure is performed under full general anesthesia, so you won’t feel anything during the surgery itself. You may feel tired and disoriented for a bit after you wake up.
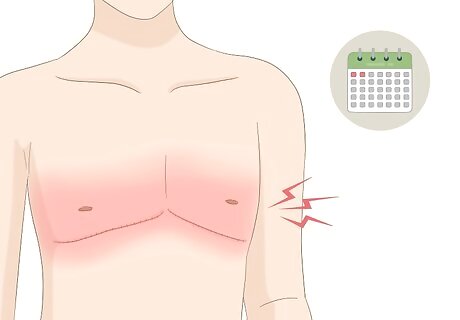
Expect some pain, swelling, and bruising in your chest. It’s normal to feel some pain, tenderness, or tightness in your chest after a chest reconstruction surgery, especially in the first 1-2 days after the procedure. You might also have some swelling and bruising, particularly during the first few weeks after the operation and you'll likely feel fatigued. If you have any concerns about what you’re seeing or feeling, don’t hesitate to call your surgeon. Use ice packs to reduce pain and swelling after your surgery. In addition, get plenty of rest, and pamper yourself following your procedure. You might continue to feel some discomfort or pain for up to 6 months after the surgery. Some people also experience numbness in their nipples or the skin of their chest. Your surgeon will prescribe medications to help manage your pain. Reach out to them right away if your pain is severe or isn’t responding to medications. However, you should be able to switch to an over-the-counter reliever within 5-7 days after the procedure, and you might not need anything within 10 days of the surgery. EXPERT TIP Scott Mosser, MD Scott Mosser, MD Board Certified Plastic Surgeon Dr. Scott Mosser is a board certified Plastic Surgeon based in San Francisco, California. Dr. Mosser is the Founder of the Gender Confirmation Center, a clinic dedicated exclusively to transgender surgeries. He received his MD from Baylor University, completed his residency in Plastic Surgery at Case Western Reserve University, and finished his fellowship in Aesthetic Surgery under Dr. John Q. Owsley, MD. He is a cofounder of the American Society of Gender Surgeons, a member of the American Society of Plastic Surgeons (ASPS), is a member of WPATH (World Professional Association of Transgender Health) and the United States Professional Association of Transgender Health (USPATH). Scott Mosser, MD Scott Mosser, MD Board Certified Plastic Surgeon Expect moderate, but not necessarily severe, pain. The amount of physical pain and emotional turmoil following a surgical procedure can be hard to gauge. However, you should be up and around shortly after having this type of procedure—patients typically report pain levels at about 3-4 on a scale of 1-10, where 10 is the most pain.
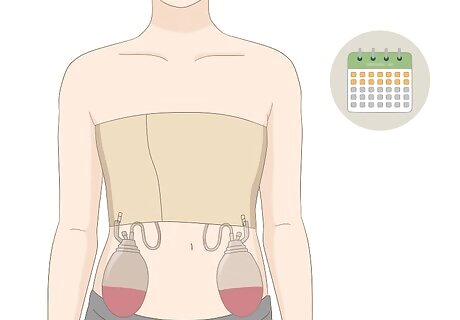
Care for your bandages and drains as recommended by your surgeon. After your surgery, you’ll need to wear an elastic compression bandage over gauze dressings for 1-2 weeks after the surgery. You’ll also most likely have a drainage tube implanted on each side of your chest to drain off excess fluids. Ask your surgeon how to care for your dressings and the drains to prevent infections and keep the surgery site clean. For example, you may need to empty the drains occasionally and record the amount of fluid that accumulates. Keep your bandages as clean and dry as possible, and don’t remove them unless your surgeon instructs you to do so. You may need to avoid bathing until your surgeon removes the bandages and drains. To keep yourself clean, use personal wipes or a damp washcloth to wipe down the rest of your body. You can also wash your hair with dry shampoo.

Sleep with your torso elevated for the first week after surgery. Sleeping with your upper body propped up can help reduce swelling and fluid buildup in your chest. Use pillows to prop up your upper body, or sleep in a recliner with your torso elevated. Your surgeon may ask you to sleep on your back to avoid putting pressure on the surgery site. Ask them when you can safely return to sleeping on your side or stomach, if that’s more comfortable for you.
Take any medications as prescribed by your surgeon. Your surgeon or doctor may prescribe medications to reduce inflammation, manage your pain, and prevent infections. If you had a nipple graft, you’ll probably need to apply antibiotic ointment to the grafts twice a day for 2-3 weeks after the surgery. Follow your doctor’s instructions for taking these medications carefully, and don’t hesitate to ask any questions you have about how to use them. Tell your surgeon about any other medications, vitamins, or supplements you’re taking before your surgery. They may ask you to stop taking certain medications or supplements to avoid complications or medication interactions.
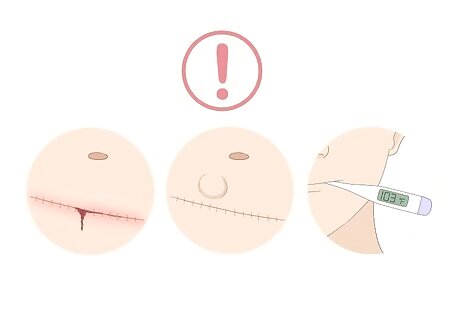
Keep an eye out for signs of infection and other complications. It’s unlikely you’ll have any major complications after your surgery, especially if you take it easy and follow your doctor’s instructions. However, problems can still occasionally come up, even if you’re taking good care of yourself. Contact your doctor right away if you notice any worrisome symptoms, such as: Severe or worsening swelling, pain, bleeding, or bruising around the surgical site Bumps or bulges under the skin on your chest An asymmetrical appearance to your chest Redness, itching, a bad smell, or unusual discharge around the surgery site A fever, chills, or a general feeling of being unwell
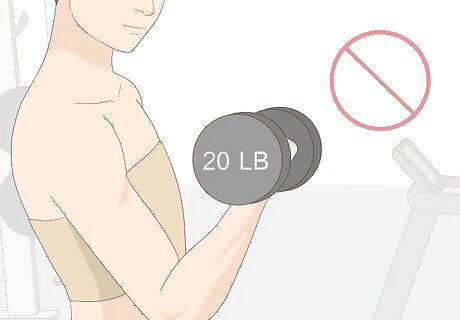
Avoid heavy lifting or strenuous activity until your surgeon says it's okay. Lifting heavy weights after your top surgery can cause damage to the incision sites and make inflammation worse. Avoid heavy pushing, intense physical activity, and lifting anything heavier than 10–15 pounds (4.5–6.8 kg) until your surgeon says it’s safe. You may need to wait 3 or 4 weeks before you can do any strenuous activity.

Avoid cigarettes or other nicotine products for at least 6 weeks after surgery. Smoking can delay your healing and make scarring worse. If you smoke, you should quit at least 2 weeks before your surgery and stay away from cigarettes for at least another 6 weeks after the surgery to achieve the best possible recovery. If you’re not sure how to quit, talk to your doctor. They can give you advice or even prescribe medications to help you quit.
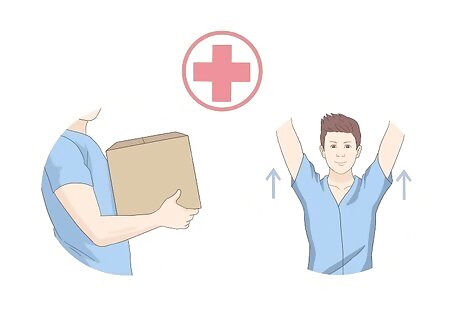
Ask when you can return to your regular activities. Resting is a crucial part of recovery after any surgery, so don’t try to jump back into your regular routine right away. Ask your surgeon when you can expect to return to activities like work, school, socializing, and getting exercise. Typically, you'll be able to resume light physical activity and sedentary work within 7-9 days after surgery, and in fact, doing so can even help the healing process. However, depending on the work you do, you should plan to take 1 1/2—2 weeks off of work, and you should avoid any physical activities that might make you sweat or increase your heart rate for about 3 weeks. After that, light cardio can be resumed, but weight training isn't recommended for at least a month. Most people can resume normal daily activities and exercise 6 months after surgery. For several types of FTM/N top surgery, you'll be advised not to lift your elbows as high as or above your shoulders for 6 months following the procedure, because that can lead to thickening and widening of the surgical scars.
Schedule follow-up appointments to check your progress. Your surgeon will want to see you a few times after the procedure to make sure you’re healing up well. Make sure you attend all of those appointments so that you can catch any issues and deal with them promptly. Let your surgeon know if you have any questions or concerns during your follow-up appointments. Individual surgeons' follow-up plans vary, but you’ll likely need to see your surgeon somewhere around 1, 2, and 6 weeks after the operation. Don’t hesitate to reach out to them or your regular doctor if you have any questions or concerns between scheduled appointments.
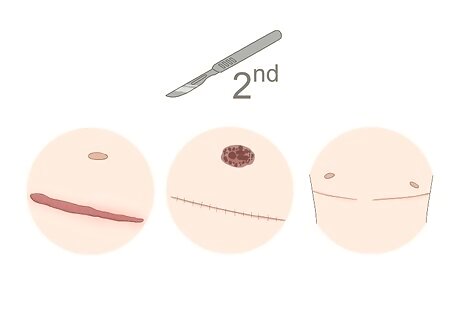
Talk to your surgeon about revision surgery if necessary. In rare cases, it might be necessary to have surgery a second time to correct any issues, such as excessive scarring, problems with your nipple graft, or an asymmetrical appearance to your chest. If you have any concerns about how your chest looks or how the surgery is healing, talk to your surgeon right away. However, also keep in mind that there are many changes in shape and swelling in the months that follow surgery, so your surgeon might not be able to assess whether a revision is necessary until 6 months after the original procedure. Some scarring is inevitable with top surgery, but you can minimize your scars by taking good care of the surgery site, avoiding smoking, and protecting the area from the sun for the first year after the surgery. EXPERT TIP Scott Mosser, MD Scott Mosser, MD Board Certified Plastic Surgeon Dr. Scott Mosser is a board certified Plastic Surgeon based in San Francisco, California. Dr. Mosser is the Founder of the Gender Confirmation Center, a clinic dedicated exclusively to transgender surgeries. He received his MD from Baylor University, completed his residency in Plastic Surgery at Case Western Reserve University, and finished his fellowship in Aesthetic Surgery under Dr. John Q. Owsley, MD. He is a cofounder of the American Society of Gender Surgeons, a member of the American Society of Plastic Surgeons (ASPS), is a member of WPATH (World Professional Association of Transgender Health) and the United States Professional Association of Transgender Health (USPATH). Scott Mosser, MD Scott Mosser, MD Board Certified Plastic Surgeon Talk to your doctor about whether you'll still need annual breast cancer screenings. Because some breast tissue will remain after top surgery, your primary care physician may still recommend that you get regularly screened for breast cancer following your procedure.
Transfeminine Top Surgery

Expect to go home the same day as the surgery. Fortunately, most people feel well enough after a breast augmentation surgery to go home the same day. You will be under general anesthesia, so you’ll likely be tired and groggy after the procedure is finished. If possible, have someone at the hospital with you who can drive you home and stay with you for the rest of the day. In breast augmentation surgery, your surgeon will insert an implant either under the skin of each breast or behind the pectoral muscle. Typically, the incisions are closed with either sutures that you cannot see, and sometimes also with surgical glue.
Be prepared for soreness, swelling, and bruising. It’s normal to feel sore for a few days after your breast augmentation surgery. You might also notice a little swelling or bruising around the incision sites. Get plenty of rest to help minimize your inflammation and discomfort. Your doctor will give you medications to help with pain and inflammation. You can also ask about using ice packs to help soothe the area. It’s normal for your bruising and swelling to get worse over the first 2-3 days after surgery before it starts to get better. As the incisions continue to heal, it’s normal to feel some itching and to experience an occasional shooting pain. However, don’t hesitate to reach out to your doctor or surgeon if you’re in a lot of pain or have any concerns about what you’re feeling.

Sleep on your back with your torso elevated. Sleeping with your upper body propped up can help reduce swelling, bruising, and fluid buildup. Pile up several pillows behind your shoulders and upper back when you sleep, or sleep in a slightly elevated recliner for a few days after your surgery. Ask your surgeon when you can safely go back to sleeping flat on your back or on your side, if that’s more comfortable for you. Avoid lying on your chest until your surgeon says it’s okay, since that can put pressure on the incision sites.
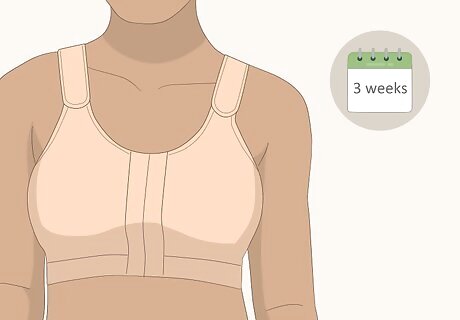
Wear a compression bra for as long as your doctor prescribes. Most surgeons recommend wearing a compression bra after breast augmentation to reduce swelling and support your healing breasts. If your surgeon recommends this, you may need to wear the bra for about 1-3 weeks after the operation.Tip: Your surgeon will likely give you the green light to take a shower as soon as 1 day after your surgery, or whenever the bandages or removed (usually a week after surgery). However, you’ll probably need to avoid swimming or soaking in a tub for at least 3 weeks. Your surgeon may provide a surgical bra, or you can wear a comfortable sports bra with a front closure. In most cases, you won’t have to wear any bandages or dressings. If your incisions are sealed with surgical glue, it should begin to fall off on its own within a few days after the procedure.
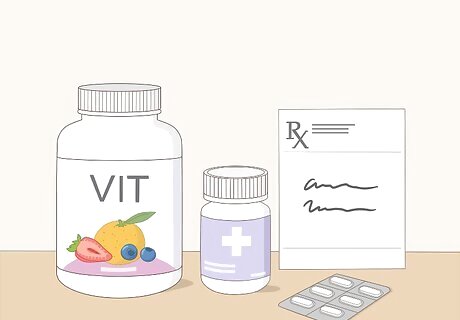
Use any medications as prescribed by your surgeon. Your surgeon may prescribe medications to reduce pain and inflammation or prevent infections. Follow the instructions for using these medications carefully, and don’t hesitate to ask any questions you may have about using them correctly. Ask your doctor before taking any non-prescribed medications or supplements after your surgery. Some of these may interact with your prescribed medications or interfere with the healing process.
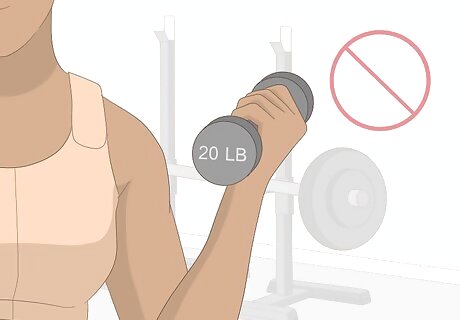
Limit upper body exercise until your surgeon says it’s okay. Avoid lifting weights over 10 pounds (4.5 kg) or doing any intense physical activity involving your upper body for at least 3 weeks after your surgery. Putting too much stress on your upper body early in the healing process can aggravate the surgical wounds or even displace the implants. It is a good idea to walk around a little bit during the first few days after the surgery if you can, since this will help promote healthy circulation in your legs. If the implants are placed beneath the muscles, most surgeons will not want you to use your chest muscles (such as doing push-ups, planking, doing Pilates, etc.) for 8 weeks after surgery.
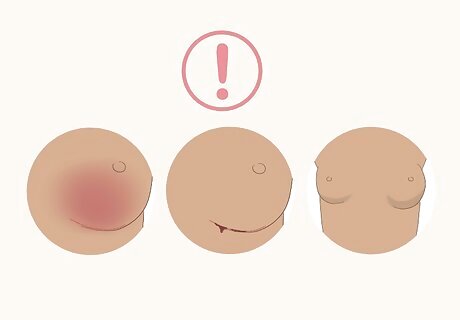
Watch for signs of infection or other complications. Serious complications after breast augmentation surgery aren’t common, but it’s still important to keep an eye out for problems. Contact your medical team right away if you have any concerns or if you notice symptoms such as: Severe swelling, pain, or redness in one or both breasts Discharge or bleeding from the surgical incisions An asymmetrical or misshapen appearance to your breasts Deflation of one of your implants Fever (as measured by a digital thermometer), chills, or a general feeling of being unwell

Don’t smoke or use any nicotine products for at least 6 weeks after the operation. Smoking can slow down the healing process and make your scars worse. If you smoke, you should quit smoking at least 2 weeks before the operation and continue to be smoke-free for at least 6 weeks after. If you’re not sure how to quit, ask your doctor for advice. You can also help minimize scarring by protecting your incisions from sunlight for at least a year after the surgery.

Discuss the milestones as to when you can return to your regular activities. Most people can return to work, school, and other regular activities about a week after surgery. However, ask your surgeon when you can safely go back. If your work or other activities are physically strenuous, you will need to wait a little longer. Rest is a very important part of the recovery process, so don’t try to jump back into your regular routines too quickly!
Attend any follow-up appointments as recommended. It’s very important to follow up with your surgeon and regular doctor after your surgery. That way, they can catch any possible issues early and take steps to correct them if necessary. You’ll likely need to see your surgeon again within 3-7 days after the surgery. Don’t hesitate to contact your doctor or surgeon if you have any questions or concerns between scheduled follow-up appointments.



















Comments
0 comment