views
X
Research source
Using the ClearBlue Fertility Monitor
Set up the monitor on days 1-4 of your first cycle. Turn on your monitor using the button at the front, then follow the on-screen instructions to set the language, calibrate the screen, and select the current date and time. After the initial setup, set a new cycle and establish a 6-hour testing window that incorporates the time of your usual first urination for the day. To set a new cycle, press the Home icon, followed by the purple dotted circle icon, followed by the dark purple dotted circle icon. Enter the date and time your period started. The first day of your cycle is the first full day of bleeding. In the context of NFP, your "first cycle" simply refers to the first cycle you track, not necessarily the first menstrual cycle you've ever had. You can also choose an optional PIN during the initial setup if desired. You'll need to enter this PIN each time you turn on the monitor if you set it.

Begin abstinence and testing on day 6. During your first cycle, the monitor will instruct you to test starting on day 6. Use a clean cup (disposable or reusable) to collect a sample from your first urination of the morning. Dip a new ClearBlue testing stick in it for 15 seconds, then remove the stick from the urine and place the cap over it. Insert the stick into the monitor with the notched-side facing down, and wait for the monitor to begin processing your test. During your first 6 cycles, you'll also need to start practicing abstinence on day 6 of your cycle to avoid pregnancy. If you're trying to achieve pregnancy, however, this isn't necessary. It'll take about 5 minutes for the monitor to process your test, and your monitor will beep when it finishes. Remove the test and check the screen. You'll see one of three readings: Low, High, or Peak. These readings indicate how fertile you are at that point in your cycle. When using the ClearBlue Monitor to assist in getting pregnant, you typically have the option of holding the testing stick under your urine stream instead of dipping it into a collected sample. When following Marquette, however, it's important that you follow the dip method instead, especially when you're trying to avoid pregnancy.
Continue testing until your peak fertility day. The monitor will ask you to continue testing until you get a Peak reading, which should happen once the monitor detects a surge of LH in your urine. The reading will change from Low to High when your estrogen increases. Your monitor will only ask you to test for a total of 20 days, and will automatically give you a Low reading on day 20 if it doesn't detect your Peak. If you don't get a Peak reading by day 19, you'll need to reset the monitor as though you're starting a new cycle. Set the cycle to day 4, then begin testing again when the monitor registers day 6. You can use supplementary LH tests in between to verify whether your LH surges in the meantime. It's best to consult a licensed Marquette instructor when learning this NFP model, especially if you have irregular cycles. For instance, if you detect a peak earlier than day 12 of your cycle or later than day 24, you'll want to consult your instructor for advice tailored to your circumstances.

Continue to observe abstinence for 3 full days after the last day of your peak (if avoiding pregnancy). A surge in LH marks the time just before ovulation, which can occur about 24-36 hours after the initial surge. It's possible to get pregnant about 3 days after an egg is released, so if you're avoiding pregnancy, you'll need to continue practicing abstinence for the 3 days following your 2-day peak. The monitor will stop asking you for a reading after your LH surge. After these 3 days pass, you're considered infertile again until day 6 of your next period. If you're trying to achieve pregnancy, your Peak days and the 3 days that follow are your most fertile days—so you probably won't want to practice abstinence on those days!
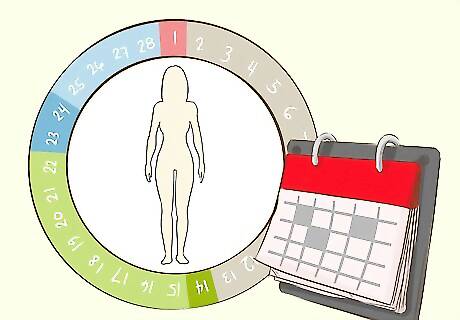
Repeat for 6 regular cycles. The menstrual cycle is a basic biological process, but every woman's cycle is unique to her in some ways. You'll need to follow the steps outlined here for the first 6 cycles so you can better understand your own pattern. It's a good idea to chart your fertility both during and after these first 6 cycles. Without charting, you won't be able to accurately track patterns.
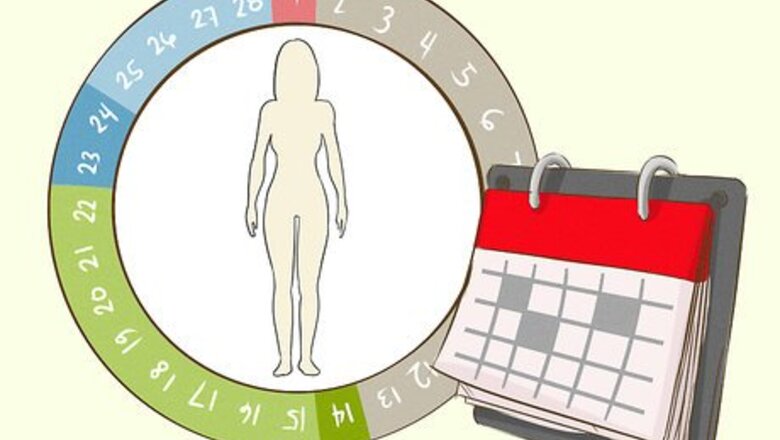
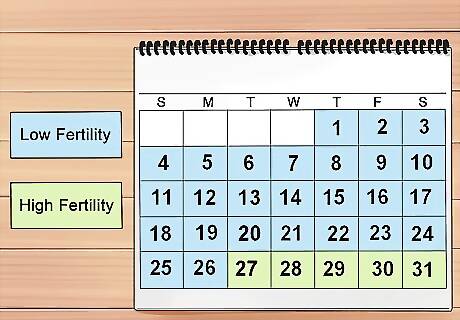
Adapt your window as needed during later cycles, but continue testing as usual. Depending on your cycle, you might consider adapting your window of abstinence if you're trying to avoid pregnancy. To limit the risk of accidentally adapting it in the wrong way, however, it's best to consult a Marquette instructor or an OB/GYN who's familiar with NFP (and the Marquette Model specifically, if possible). Your situation may vary, but generally, you'll calculate your fertile window based on the earliest day of ovulation during the first 6 months. Your biological fertile window lasts for about 6 days. Sperm can live for about 5 days. Set your fertility window 6 days before the earliest peak of the past 6 cycles. For example, if your earliest peak day was day 14, your fertility window starts on day 8. It's important to continue testing as usual, however. If you get a High reading before the estimated start date for your fertility window, you should consider yourself fertile at that point. You'll also need to recalculate your fertility window after each cycle. Always adjust your window based on the past 6 cycles.
Tracking Your Cervical Mucus

Check your cervical mucus every day, throughout the day. At a minimum, you should check changes to your cervical mucus at least 2-3 times per day, but checking every time you use the bathroom will provide more accurate data. Wipe before and after urinating and look at the tissue to observe changes in appearance and amount. You may also consider feeling it between your fingers to get a better understanding of the texture and quality. Record only your most fertile mucus for the day, even if you check multiple times per day. You could technically follow the Marquette Model using the monitor only, but tracking urine hormone readings alongside changes to your cervical mucus will increase the method's effectiveness and help you better understand your body.
Expect little or no mucus during the early days of your cycle. Don't worry about checking for mucus during your period—you're infertile during that part of your cycle. Even after your period, you may experience several days of dryness or very little mucus. These days generally correspond to the infertile parts of your cycle. Immediately following your days of dryness, you may notice thick, white mucus that holds its shape. This type of mucus is also generally a sign of low fertility.

Look for damp, slightly stretchy mucus on high fertility days. When you notice an increase in wet cervical mucus, you've likely transitioned into a stage of high fertility. This mucus looks thinner and slightly stretchy, and may also be somewhat cloudy. You'll definitely need to abstain from sex during this stage if you're trying to avoid pregnancy. This stage will usually overlap with High fertility readings on your monitor, but don't be too alarmed if the fertility windows between both data sets don't perfectly match. There are several reasons why this may happen. Consult with a Marquette instructor or OB/GYN to narrow down what might cause this in your own cycle.

Observe abundant, slippery mucus during peak fertility. Mucus that occurs during your peak fertility days will be abundant and very slippery. It looks a little like raw egg white: thin, clear, and watery/stretchy.
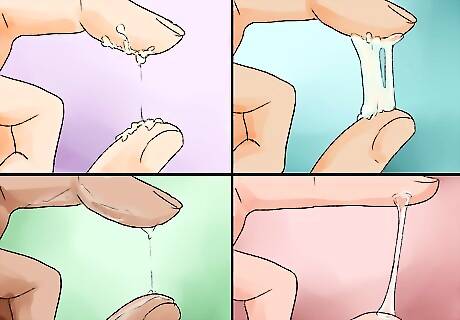
Verify the return of low fertility mucus after your peak. After your peak days, you'll notice less cervical mucus again. It might seem tacky and cloudy, or it might return to being completely dry again.
Factor this information into your fertility window. When you start recalculating your fertility window after the first 6 cycles, you should also consider what your body is telling you through your cervical mucus. If your monitor and mucus readings don't agree about when your fertility window starts, base your calculation on the earliest possible start point. For example, if your earliest peak day according to the monitor was day 14, but your peak mucus reading first occurred on day 13, count back 6 days from day 13 to find the start date of your fertility window (day 7).
Checking Supplementary Signs
Track your Basal Body Temperature (BBT) to confirm ovulation. Using a digital BBT thermometer, start taking your temperature every morning as soon as you wake up and before you get out of bed. Try to take your temperature within the same 30-minute window each day, and take it orally. Chart your temperature each day and look for patterns. Generally, your temperature will increase at least 0.4 degrees over a 48-hour period when you ovulate.
Use progesterone tests as another way to confirm ovulation. There are several home urine tests you can use to confirm an increase in progesterone, which happens after one of your ovaries releases an egg. Collect a urine sample first thing in the morning and place the testing strip into the sample for 5-10 seconds (or whatever length of time your specific test kit says). After about 5 minutes, the strip should indicate whether you've tested positive or negative for progesterone. A positive result means you've ovulated. If you decide to test progesterone, begin 3 days after your peak and continue testing until you get a positive result or as instructed by the testing kit.
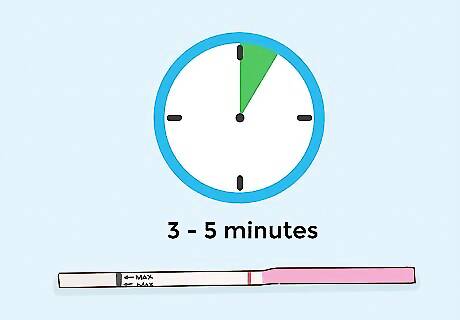
Take separate LH tests (OPKs) to confirm your peak fertility. If you need to reset the cycle on your monitor (e.g., as you would if your cycle extends past 19 testing days) or if you're unable to test with the monitor during the testing window you previously set, you can use a separate LH test, also called an Ovulation Predictor Kit (OPK) You can also use these tests alongside the monitor if you're concerned you may miss your LH surge with the monitor. Test daily in the afternoon, starting on cycle day 6. You should ideally have 3-4 hours worth of urine in your bladder before testing. You'll usually need to collect a sample of urine, dip a test strip into it for around 5 seconds, and check the results within 3-5 minutes.
Putting the Details Together
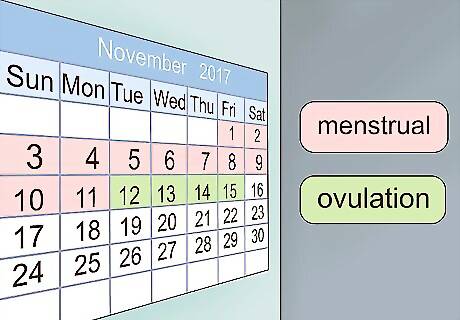
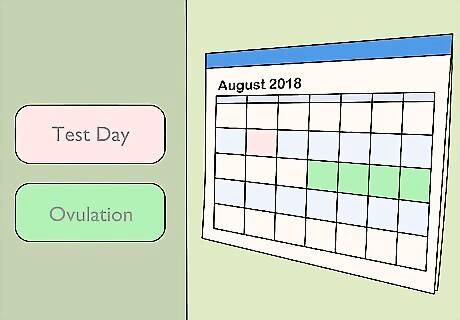
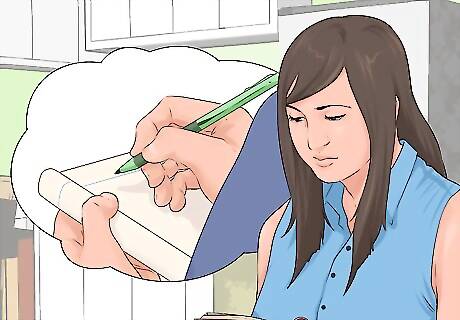
Maintain accurate charts. You can use a paper chart, a spreadsheet on your computer, a calendar, or a fertility app. Note of all the biomarkers you've been tracking using this chart, and update your chart daily to avoid forgetting important information. If you're tracking BBT in addition to the monitor and mucus results, you may consider making a separate line graph to help you visually track when your BBT spikes upward.

Know that the Marquette Model can be used to help avoid or achieve pregnancy. Because NFP teaches you how to be aware of your menstrual cycle and work with it, you can use it to help you either avoid pregnancy or achieve it. This is true of the Marquette Model, as well as every other method of practicing NFP. Set your intention—avoid or achieve—at the start of each cycle so you'll know what to do (and not do) as your cycle progresses. As a general rule, avoid sex during high and peak fertility parts of your cycle if you're trying to avoid pregnancy. If you're trying to achieve pregnancy, however, these will be the best days to have sex.
Observe periods of abstinence to improve the effectiveness rate when avoiding. This is nobody's favorite part of NFP, but if you're sincerely trying to avoid pregnancy, it's best to practice abstinence during your fertile window. Hormonal birth control can't be used during selective portions of your cycle—you have to use it continually for it to affect your hormones—and the most common barrier methods of birth control are only about 71-88% effective at preventing pregnancy with typical use. The withdrawal method is only 78% effective. Abstaining from sex during your fertile window will improve your odds of success when trying to avoid pregnancy with Marquette. If you're practicing NFP for faith-based reasons, that might be another reason to avoid contraceptives and stick with periods of abstinence. For instance, the Catholic Church officially approves the Marquette Model, but also teaches against the use of contraceptives. If you have questions about your faith's teachings regarding contraceptives—whether you're confused about what those teachings are or what the theological reason is behind them—consult a Marquette instructor or faith leader.

Consult a Marquette Model instructor to improve effectiveness rates for avoiding or achieving. All Marquette instructors are healthcare providers with a minimum Bachelor of Science in Nursing. Instructors will work with you to help you better understand the process, and most will offer follow-ups and additional support via phone or email if you have questions. You can work with an in-person or online instructor. Start by searching the official directory: https://www.marquettemethod.com/instructors/ Every woman practicing the Marquette Model will benefit from formal instruction, but this can be especially important if you have an irregular cycle, a reproductive disorder, or other special concerns.

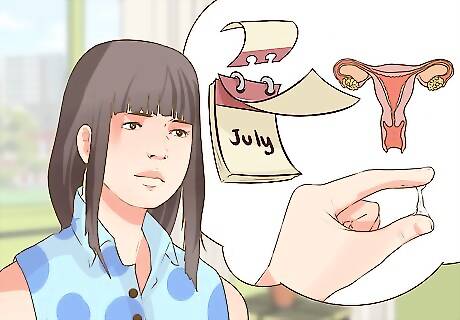
Recognize how the Marquette Model may vary if you don't have regular cycles. An average menstrual cycle lasts 21 to 35 days. However, certain conditions and disorders (e.g., polycystic ovary syndrome, pelvic inflammatory disease, and uterine fibroids, among others) can cause your cycle to be shorter or longer. You might have to take a few extra steps to ensure accurate testing and charting if your cycle is irregular. For regular cycles, ovulation typically occurs between cycle days 10 and 20. Women with shorter cycles may need to begin testing and periods of abstinence prior to day 6, and women with longer cycles may need to test longer. In some cases, you'll even need to reset the monitor and begin retesting after cycle day 24. More testing could mean a higher expense, as well as more days of abstinence when you're trying to avoid pregnancy. Work with your NFP instructor to determine how your irregular cycle changes the way you practice NFP, and the Marquette Model in particular. You should also consult your OB/GYN to determine the cause of your cycle irregularities if you don't already know.
















Comments
0 comment