views
Managing Clots
Seek medical attention immediately if you suspect a blood clot in your lungs. Blood clots that form in the veins in your arms, legs, and groin could break loose and move to your lungs, which is called a pulmonary embolism. If the clot moves to your lungs, it could be life-threatening, so call emergency services or visit an emergency room right away. Signs of a blood clot in your lungs include difficulty breathing, chest pain, elevated heart rate, mild fever, coughing with or without blood, and fainting spells.
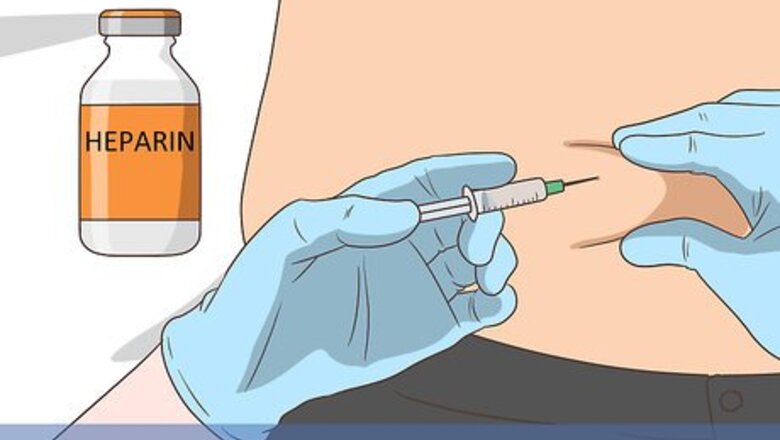
Begin with heparin. Keep your arm elevated to help you reduce pain and swelling. Your treatment will probably start with an injection or IV of the anticoagulant, heparin. Side effects of heparin include bleeding, bruising, rash, headache, common cold symptoms, and nausea.
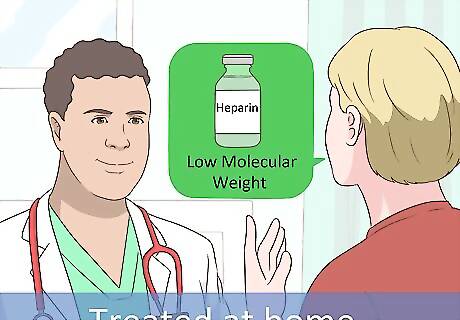
Ask your doctor about taking low molecular weight heparins. If you'll be treated at home instead of at the hospital, ask your doctor about low molecular weight heparins. These injections can be given at home without the need for frequent blood tests. Low molecular weight heparins are expensive, so standard heparins are more commonly given.
Take warfarin by mouth. Unlike heparin, the anticoagulant warfarin takes longer to work so the doctor will probably have you begin the warfarin while you get heparin injections. Once the warfarin pills begin working, the doctor will stop the heparin and you can leave the hospital. Follow your doctor's treatment plan for taking warfarin once you get home. Depending on the cause of your clot, you may need to take warfarin for a few weeks or the rest of your life.

Get regular blood testing. After you've been following your doctor's treatment plan at home, you'll need to return to the hospital for blood work. You'll need blood testing 2 to 3 times a week starting out. The doctor will check your blood to see how long it takes to clot. Eventually, you may be able to go up to 4 weeks in between blood tests.
Trying Alternatives to Medication
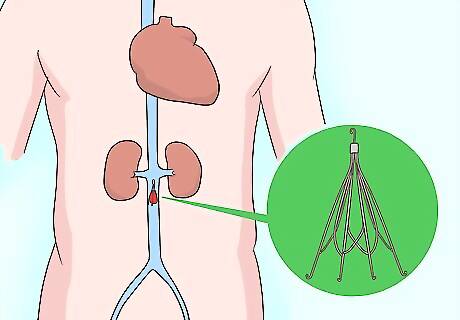
Get surgery to insert a filter into a large vein. If you can't take anticoagulant medications or they aren't working, a surgeon will insert a small mesh filter into 1 of the largest veins in your body. This filter should catch blood clots before they get to your heart or lungs. If you have a very large clot that's causing tissue damage, a surgeon may perform an emergency thrombectomy. For this procedure, the surgeon will cut into the vein in your arm to remove the clot.

Keep your arm elevated and wear compression sleeves. Buy compression sleeves from a pharmacy or wellness center. These are made of elastic that will feel tight against your arm near the wrist but loose towards your shoulder. The compression sleeve will reduce swelling and improve circulation in your arm.
Eat a low-fat, high-fiber diet to prevent DVT. Reduce the amount of cholesterol and saturated fats you’re eating since they can put you more at risk for blood clots. Instead, try a low-fat, vegetarian, or vegan diet to help you stay healthy. Do your best to avoid red or processed meats since they could increase your chances of forming clots. Try to incorporate 5 servings of fruits and vegetables every day. Stay hydrated by drinking 8 glasses of water every day as well. Incorporate garlic, turmeric, and vitamin E supplements into your diet, but talk to your doctor if you’re already on anticoagulant therapy.

Contact your doctor if your DVT worsens. If you think you're experiencing side effects to any of your medications or your arm begins feeling worse, call your doctor or nurse. Get immediate medical attention by calling emergency services or going to an emergency room if you notice any of the following: New or returning pain in either of your arms Severe headaches that don't go away Blood in your nose, gums, urine, mucus, or vomit Bruising that doesn't heal
Recognizing and Diagnosing DVT

Check your arm for pain or swelling which could indicate a blood clot. DVT can cause swelling and tenderness in your arm. You might also feel pain and see that part of your arm is red. This pain and irritation may be sudden instead of gradual. Other signs of DVT include: Difficulty moving your arm Warm skin over the painful area Heavy ache in your arm

Schedule an exam with your doctor. If you have any signs of a clot in your arm, contact your doctor for an immediate physical exam. The doctor will take your medical history, look at your arm, and consider your risk for developing DVT. Recent research suggests that DVT is a chronic condition, so if you've experienced clotting in the past, you may be more likely to develop another clot. Some other risk factors for DVT include: Pregnancy Recent hospitalization or surgery Physical inactivity Prolonged sitting or laying Obesity Hormone therapy Smoking Vitamin D deficiency Taking birth control pills Traumatic brain injury Cancer
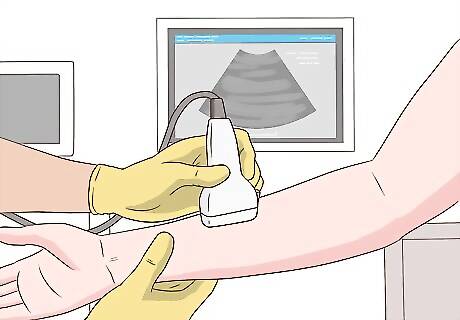
Get an ultrasound to confirm a DVT diagnosis. If the doctor suspects you have DVT, they'll do an ultrasound of your arm. The ultrasound can show blockages or clots deep within the veins of your arm. Although MRIs and CT scans can also show your veins and clots, they're not usually used to diagnose DVT.
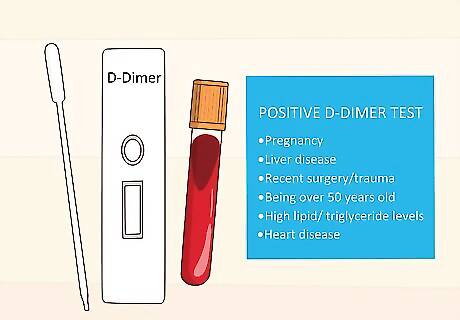
Do a D-dimer blood test. If the doctor doesn't see blockages or clots in your ultrasound, they may take a sample of your blood for testing. They'll examine the blood for signs that blood clots are breaking up. If the test comes back negative, you probably don't have DVT. Keep in mind that several factors may result in a positive D-dimer test including: Pregnancy Liver disease Recent surgery or trauma Being over 50 years old High lipid or triglyceride levels Heart disease
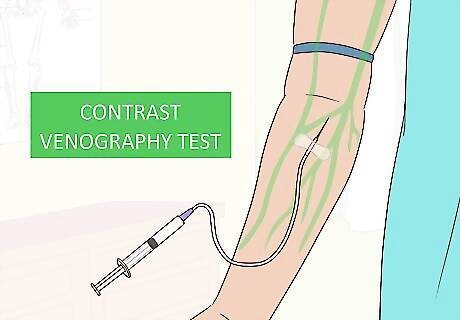
Ask for a contrast venography test. The doctor may want to do a more invasive but accurate test if they're still unsure if you have DVT in your arm. They'll inject dye into a big vein in your arm to see how easily the blood and dye travels throughout your veins.


















Comments
0 comment