
views
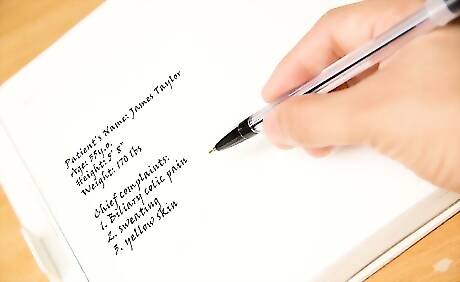
Take down the patient's name, age, height, weight and chief complaint or complaints.

Gather the primary history. Ask the patient to expand on the chief complaint or complaints. In particular, ask about anything that the patient was unclear about or that you don't understand. Get specific numbers for things like how long the patient has had the symptoms or how much pain, on a scale of 0 to 10, the patient is experiencing. Record, as accurately as you can, what the patient tells you. Don't add your interpretation to what you hear.

Expand with the secondary history. This is where you ask about any symptoms the patient is experiencing that are related to the chief complaint. Associated symptoms are often the key to making a correct diagnosis. The patient may not recognize that associated symptoms are related to the chief complaint and may not even view them as symptoms. You will have to interpret what you hear to complete this section of the medical history.
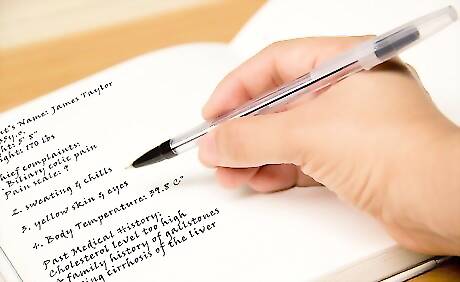
Take the tertiary history. This is anything in the patient's past medical history that may have something to do with the current chief complaint. By this point, you may already be fairly certain about the diagnosis, so you can home in on specific problems or events that support it.

Include a review of symptoms. This is simply a list, by area of the body, of anything that the patient feels might not be normal. It's best to have the list of body areas in mind as you question the patient so you don't forget to ask about each one. Question the patient about these areas: General constitution Skin and breasts Eyes, ears, nose, throat and mouth Cardiovascular system Respiratory system Gastrointestinal system Genitals and urinary system Musculoskeletal system Neurological or psychological symptoms Immunologic, lymphatic and endocrine system
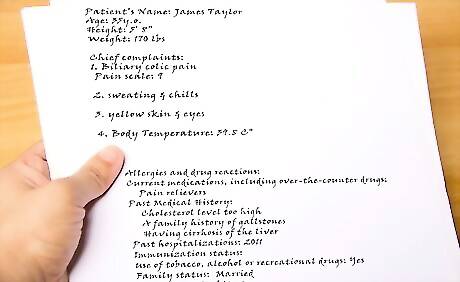
Interview the patient for a past medical history. This is background information on anything having to do with the patient's health, not just the current chief complaint. At a minimum it should include the following, but be prepared to take down any information the patient gives you that might be relevant: Allergies and drug reactions Current medications, including over-the-counter drugs Current and past medical or psychiatric illnesses or conditions Past hospitalizations Immunization status Use of tobacco, alcohol or recreational drugs Reproductive status (if female), including date of last menstrual period, last gynecological exam, pregnancies and contraception method Information on children Family status, including whether the patient is married, who the patient lives with and other relationships. Include questions about the patient's current sexual activity and history. Occupation, particularly if it includes exposure to hazardous materials


















Comments
0 comment